Low-Risk Recovery Fees for platform services are primarily based on a contingency fee model, which means Providers pay Curae when new revenue is gained.
A Comprehensive Revenue Cycle Management Platform for Providers
Easily integrates with your ecosystem and processes to reduce uncompensated care and improve the patient experience.
Financial Improvement Potentially Gained With Our Patient Financial Access Platform
Increase Revenue by Covering More Patients
Enable care for uninsured patients and fund high-cost essential drug therapies for those denied coverage.*
Optimize Cash Flow Through RCM Precision
Shorten the revenue cycle and reduce A/R aging with data-driven workflows that accelerate collections and unlock trapped cash.*
Achieve a Quick Return on Decision
Start seeing new revenue and cash flow within 8-12 weeks typically from contract execution, providing financial improvements to your health system.*
Strengthen Operational Efficiency
Automate follow-up, streamline billing, and reduce costly rework—freeing up staff time while increasing financial yield across the revenue cycle.*
Increase Your Net Promoter Score (NPS) by 30 Points
Improve the patient journey with CURAE’s platform, designed to streamline financial processes, enhance satisfaction, and elevate your healthcare system’s reputation.*
*Results may vary. Based on internal data research.
Our Solutions
CURAEClear
Identify insurance coverage at the time of service, with superior identification rates for rebilling and ongoing processes. Discover Medicare Underpayment Recovery and Transfer DRG.
CURAEAdvocate
Enroll eligible patients in ACA plans to gain coverage for complex procedures/therapies.
CURAE– EBO
Optimize revenue cycle management with intelligent, automated solutions.

What makes our platform different?
Risk-Free Recovery
State-of-the-Art Technology
Powered by proprietary algorithms, enabling the processing of large, complex data files with unmatched efficiency.
Rapid Implementation
Integrates seamlessly into your existing workflows, with a simple implementation process.
Unmatched Results
A World-Class Platform
Designed to support the financial journey, improve the patient experience, and bolster your healthcare system’s brand.
Automated Insurance Eligibility Checks:
To efficiently identify coverage options for patients.
Underpayment Auditing:
Advanced algorithms to detect and recover due payments.
Comprehensive Data Analytics:
To leverage over 40 billion data points for informed decision-making.

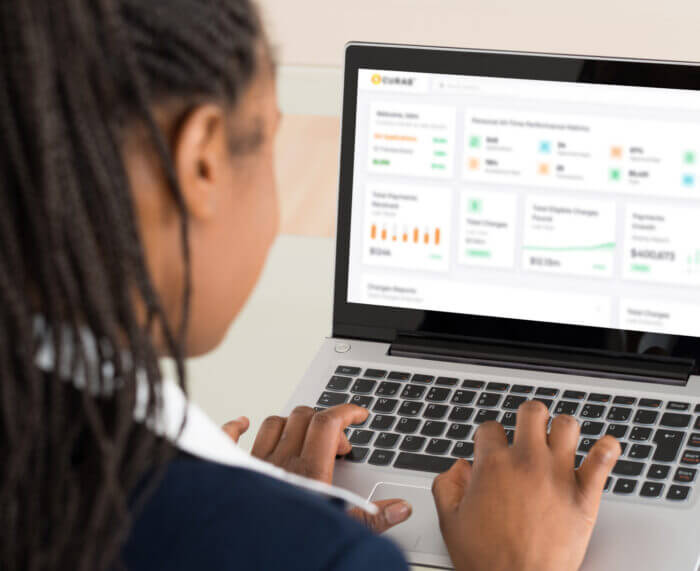
See Our Platform in Action
Discover how CURAE’s platform can transform your healthcare system by improving patient satisfaction, streamlining billing processes, and increasing revenue.